 Home
Home
December 21, 2023
Fosfomycin for treating lower urinary tract infection (UTI)
A group home owner is requesting antibiotics for a hospice patient who’s been increasingly confused over the last several days and has foul smelling urine. You order a culture & sensitivity (C&S) that reveals bacterial growth in the urine and resistance to multiple antibiotics. The susceptible antibiotics listed on the report aren’t ideal because they require IM injection (painful), IV infusion (often impractical and possibly costly), laboratory monitoring, or have been ruled out due to allergies.
This scenario isn’t uncommon and can be frustrating. Nonspecific symptoms and bacteriuria are poor predictors of urinary tract infection (UTI) in older adults, but hospice providers may be compelled to order antibiotics for one reason or another. So what can they prescribe when options are limited? Fosfomycin might be a practical choice, especially if oral antibiotics are preferred.
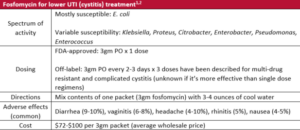
Fosfomycin was discovered in the late 1960s and despite being used throughout Europe for many years, it wasn’t introduced in the US until 1996.1,2 It’s a broad-spectrum antibiotic in a class of its own that has activity against various gram-positive and gram-negative organisms. Notably, it has excellent activity against E. coli, the organism primarily responsible for UTIs, and there’s evidence of efficacy for treating multidrug-resistant organisms (including ESBL–E. coli) that might otherwise call for parenteral antibiotics.3
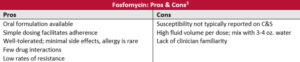
Fosfomycin is only FDA-approved for treating uncomplicated lower UTI (cystitis), which by definition excludes patients who are male or have indwelling catheters, but there’s encouraging data to support its use for complicated UTI as well.3 It isn’t recommended for upper UTI involving the kidney (pyelonephritis) because of its poor ability to concentrate in the upper urinary tract.1
Fosfomycin susceptibility isn’t routinely included on culture and sensitivity reports because recommended methods are labor and time intensive and reporting standards are poorly defined, but providers can ask about it since some labs can complete this testing by request.4 Still, fosfomycin shouldn’t be ruled out as a potentially useful antibiotic for treating lower UTI.
Written by: OnePoint Patient Care Clinical Team
Joseph Solien, PharmD, BCGP, BCPP – Vice President of Clinical Services
Melissa Corak, PharmD, BCGP – Senior Clinical Pharmacist
John Corrigan, PharmD, BCGP – Clinical Pharmacist
References
- Gardiner B, et al. Nitrofurantoin and Fosfomycin for Resistant Urinary Tract Infections: Old Drugs for Emerging Problems. Aust Prescr. 2019;42:14-19. doi:10.18773/austprescr.2019.002
- Lexi-Comp
- Derington C, et al. Multiple-Dose Oral Fosfomycin for Treatment of Complicated Urinary Tract Infections in the Outpatient Setting. Open Forum Infect Dis. 2020;7(2):ofaa034. doi:10.1093/ofid/ofaa034
- Smith E, at al. Performance of Four Fosfomycin Susceptibility Testing Methods against an International Collection of Clinical Pseudomonas aeruginosa Isolates. J Clin Microbiol. 2020;58(10):e01121-e01120. doi:10.1128/JCM.01121-20